Accuracy of Fetal Heart Rate Acquired from Sensors on the Maternal Abdomen Compared to a Fetal Scalp Electrode

Objective:
To compare fetal heart rate measured using electrodes on the maternal abdomen to the fetal rate acquired using the fetal scalp electrode (FSE).
Methods:
Data were acquired from 27 term
laboring women who had a FSE placed for a clinical indication. 29 channels of abdominal data and one chest lead were recorded simultaneously with the FSE. The data were preprocessed for removal of interference from maternal ECG as well as power‐line contamination and other sources of background noise, such as muscle artifact.
Methods (cont'd):
Signal quality measures were used to select regions of usable data from both the scalp and abdominal electrodes. A total of 542 10‐second segments,
sampled every 30 seconds, were
chosen from the FSE and the
preprocessed abdominal data.
The associated median fetal heart rate was calculated in each segment of the abdominal and scalp data. A statistical
comparison between the fetal heart rate calculated in simultaneous segments of abdominal and scalp data was performed. This allowed us to access the accuracy of the fetal heart rate recorded from abdominal sensors compated to the "gold standard," FSE.
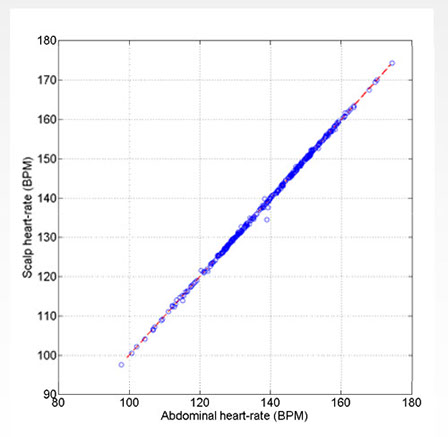
Results:
The fetal heart rate was successfully extracted from the FSE from 85.6 percent of analyzed segments, and 83.3 percent of analyzed segments recorded using abdominal sensors.
The root mean square error between the fetal heart rate sequence calculated by both methods averaged over all processes segments was 0.35 beat per minute.
Conclusion:
FHR acquired from the maternal abdomen is highly accurate and on average is clinically indistinguishable from FHR calculated using the fetal scalp electrode data. Furthermore, using our method, abdominal fetal ECG is useful for FHR estimation almost as often as data
from scalp electrode data. Our method can be used as a reliable alternative to the FSE for automated FHR reporting and noisy data rejection.
Reza Sameni PhD 1,2 Gari Clifford PhD 2,3,4 Ward Sameni, PhD, Clifford, PhD, Jay Ward,2 Jim Robertson,2 Courtenay Pettigrew,5 Adam J. Wolfberg, MD, MPH,2,5,6
1Shiraz University, 2MindChild Medical, Inc., 3Massachusetts Institute of Technology, 4Oxford University, 5Tufts Medical Center, 6Children’s Hospital, Boston
Disclosure: The authors, except for Ms. Pettigrew, hold equity in MindChild Medical, Inc., which has licensed intellectual property used to generate results presented in this abstract.
© 2021-2022 Mindchild Medical, Inc. | 1600 Osgood Street | Suite 2017 | North Andover, MA 01845 | info@mindchild.com | 978.566.9880